Abstract
Background
Sexual assault and/or sexual harassment during military service (military sexual trauma (MST)) can have medical and mental health consequences. Most MST research has focused on reproductive-aged women, and little is known about the long-term impact of MST on menopause and aging-related health.
Objective
Examine associations of MST with menopause and mental health outcomes in midlife women Veterans.
Design
Cross-sectional.
Participants
Women Veterans aged 45–64 enrolled in Department of Veterans Affairs (VA) healthcare in Northern California between March 2019 and May 2020.
Main Measures
Standardized VA screening questions assessed MST exposure. Structured-item questionnaires assessed vasomotor symptoms (VMS), vaginal symptoms, sleep difficulty, depressive symptoms, anxiety symptoms, and posttraumatic stress disorder (PTSD) symptoms. Multivariable logistic regression analyses examined associations between MST and outcomes based on clinically relevant menopause and mental health symptom thresholds.
Key Results
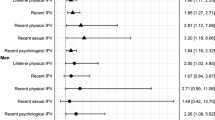
Of 232 participants (age = 55.95 ± 5.13), 73% reported MST, 66% reported VMS, 75% reported vaginal symptoms, 36% met criteria for moderate-to-severe insomnia, and almost half had clinically significant mental health symptoms (33% depressive symptoms, 49% anxiety, 27% probable PTSD). In multivariable analyses adjusted for age, race, ethnicity, education, body mass index, and menopause status, MST was associated with the presence of VMS (OR 2.44, 95% CI 1.26–4.72), vaginal symptoms (OR 2.23, 95% CI 1.08–4.62), clinically significant depressive symptoms (OR 3.21, 95% CI 1.45–7.10), anxiety (OR 4.78, 95% CI 2.25–10.17), and probable PTSD (OR 6.74, 95% CI 2.27–19.99). Results did not differ when military sexual assault and harassment were disaggregated, except that military sexual assault was additionally associated with moderate-to-severe insomnia (OR 3.18, 95% CI 1.72–5.88).
Conclusions
Exposure to MST is common among midlife women Veterans and shows strong and independent associations with clinically significant menopause and mental health symptoms. Findings highlight the importance of trauma-informed approaches to care that acknowledge the role of MST on Veteran women’s health across the lifespan.

Similar content being viewed by others
References
Wilson LC. The prevalence of military sexual trauma: a meta-analysis. Trauma Violence Abuse. 2018;19(5):584-597. https://doi.org/10.1177/1524838016683459
Hargrave AS, Maguen S, Inslicht SS, et al. Veterans Health Administration screening for military sexual trauma may not capture over half of cases among Midlife Women Veterans. Women’s Health Issues. 2022;32(5):509-516. https://doi.org/10.1016/j.whi.2022.06.002
Kimerling R, Gima K, Smith MW, Street A, Frayne S. The Veterans Health Administration and Military Sexual Trauma. Am J Public Health. 2007;97(12):2160-2166. https://doi.org/10.2105/AJPH.2006.092999
Frayne SM, Skinner KM, Sullivan LM, et al. Medical profile of Women Veterans Administration outpatients who report a history of sexual assault occurring while in the military. J Womens Health Gend Based Med. 1999;8(6):835-845. https://doi.org/10.1089/152460999319156
Maguen S, Luxton DD, Skopp NA, Madden E. Gender differences in traumatic experiences and mental health in active duty soldiers redeployed from Iraq and Afghanistan. J Psychiatr Res. 2012;46(3):311-316. https://doi.org/10.1016/j.jpsychires.2011.11.007
Kimerling R, Street AE, Pavao J, et al. Military-related sexual trauma among Veterans Health Administration patients returning from Afghanistan and Iraq. Am J Public Health. 2010;100(8):1409-1412. https://doi.org/10.2105/AJPH.2009.171793
Goldstein LA, Dinh J, Donalson R, Hebenstreit CL, Maguen S. Impact of military trauma exposures on posttraumatic stress and depression in female veterans. Psychiatry Res. 2017;249:281-285. https://doi.org/10.1016/j.psychres.2017.01.009
Blais RK, Brignone E, Maguen S, Carter ME, Fargo JD, Gundlapalli AV. Military Sexual Trauma is associated with post-deployment eating disorders among Afghanistan and Iraq veterans: BLAIS et al. Int J Eat Disord. 2017;50(7):808-816. https://doi.org/10.1002/eat.22705
Cohen BE, Maguen S, Bertenthal D, Shi Y, Jacoby V, Seal KH. Reproductive and other health outcomes in Iraq and Afghanistan Women Veterans using VA Health Care: association with mental health diagnoses. Womens Health Issues. 2012;22(5):e461-471. https://doi.org/10.1016/j.whi.2012.06.005
Pulverman CS, Christy AY, Kelly UA. Military Sexual Trauma and sexual health in Women Veterans: a systematic review. Sex Med Rev. 2019;7(3):393-407. https://doi.org/10.1016/j.sxmr.2019.03.002
Pulverman CS, Creech SK. The impact of sexual trauma on the sexual health of women Veterans: a comprehensive review. Trauma Violence Abuse. 2021;22(4):656-671. https://doi.org/10.1177/1524838019870912
Ryan GL, Mengeling MA, Booth BM, Torner JC, Syrop CH, Sadler AG. Voluntary and involuntary childlessness in female Veterans: associations with sexual assault. Fertil Steril. 2014;102(2):539-547. https://doi.org/10.1016/j.fertnstert.2014.04.042
DiMauro J, Renshaw KD, Blais RK. Sexual vs. non-sexual trauma, sexual satisfaction and function, and mental health in female Veterans. J Trauma Dissociation. 2018;19(4):403-416. https://doi.org/10.1080/15299732.2018.1451975
Turchik JA, Pavao J, Nazarian D, Iqbal S, McLean C, Kimerling R. Sexually transmitted infections and sexual dysfunctions among newly returned Veterans with and without military sexual trauma. Int J Sexual Health. 2012;24(1):45-59. https://doi.org/10.1080/19317611.2011.639592
Pavao J, Turchik JA, Hyun JK, et al. Military sexual trauma among homeless Veterans. J Gen Intern Med. 2013;28 Suppl 2:S536-541. https://doi.org/10.1007/s11606-013-2341-4
Mattocks KM, Sadler A, Yano EM, et al. Sexual victimization, health status, and VA Healthcare Utilization among lesbian and bisexual OEF/OIF Veterans. J Gen Intern Med. 2013;28 Suppl 2:S604-608. https://doi.org/10.1007/s11606-013-2357-9
Calhoun PS, Schry AR, Dennis PA, et al. The Association between Military Sexual Trauma and use of VA and Non-VA Health Care services among female veterans with military service in Iraq or Afghanistan. J Interpers Violence. 2018;33(15):2439-2464. https://doi.org/10.1177/0886260515625909
Gibson CJ, Maguen S, Xia F, Barnes DE, Peltz CB, Yaffe K. Military sexual trauma in older women Veterans: prevalence and comorbidities. J Gen Intern Med. 2020;35(1):207-213. https://doi.org/10.1007/s11606-019-05342-7
Cook JM, Dinnen S, O’Donnell C. Older women survivors of physical and sexual violence: a systematic review of the quantitative literature. J Womens Health (Larchmt). 2011;20(7):1075-1081. https://doi.org/10.1089/jwh.2010.2279
Katon JG, Rodriguez A, Yano EM, et al. Research priorities to support Women Veterans’ Reproductive Health and health care within a learning health care system. Women’s Health Issues. Published online January 2023:S1049386722001797. https://doi.org/10.1016/j.whi.2022.12.003
Gibson CJ, Huang AJ, McCaw B, Subak LL, Thom DH, Van Den Eeden SK. Associations of intimate partner violence, sexual assault, and posttraumatic stress disorder with menopause symptoms among midlife and older women. JAMA Intern Med. 2019;179(1):80-87. https://doi.org/10.1001/jamainternmed.2018.5233
Tracy EE, Speakman E. Intimate partner violence: not just a concern of the reproductive ages. Menopause. 2012;19(1):3-5. https://doi.org/10.1097/gme.0b013e318239c985
Gold EB, Sternfeld B, Kelsey JL, et al. Relation of demographic and lifestyle factors to symptoms in a multi-racial/ethnic population of women 40-55 years of age. Am J Epidemiol. 2000;152(5):463-473. https://doi.org/10.1093/aje/152.5.463
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606-613. https://doi.org/10.1046/j.1525-1497.2001.016009606.x
Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092. https://doi.org/10.1001/archinte.166.10.1092
Bastien CH, Vallières A, Morin CM. Validation of the Insomnia Severity Index as an outcome measure for insomnia research. Sleep Med. 2001;2(4):297-307. https://doi.org/10.1016/s1389-9457(00)00065-4
Green R, Santoro N. Menopausal symptoms and ethnicity: the study of women’s health across the Nation. Womens Health (Lond Engl). 2009;5(2):127-133. https://doi.org/10.2217/17455057.5.2.127
Im EO, Chang SJ, Chee E, Chee W. The relationships of multiple factors to menopausal symptoms in different racial/ethnic groups of midlife women: the structural equation modeling. Women Health. 2019;59(2):196-212. https://doi.org/10.1080/03630242.2018.1450321
Minkin MJ, Reiter S, Maamari R. Prevalence of postmenopausal symptoms in North America and Europe. Menopause. 2015;22(11):1231-1238. https://doi.org/10.1097/GME.0000000000000464
Santoro N, Komi J. Prevalence and impact of vaginal symptoms among postmenopausal women. J Sex Med. 2009;6(8):2133-2142. https://doi.org/10.1111/j.1743-6109.2009.01335.x
Soares CN. Mood disorders in midlife women: understanding the critical window and its clinical implications. Menopause. 2014;21(2):198-206. https://doi.org/10.1097/GME.0000000000000193
Thurston RC, Bromberger JT, Joffe H, et al. Beyond frequency: who is most bothered by vasomotor symptoms? Menopause. 2008;15(5):841-847. https://doi.org/10.1097/gme.0b013e318168f09b
Avis NE, Crawford SL, Greendale G, et al. Duration of menopausal vasomotor symptoms over the menopause transition. JAMA Intern Med. 2015;175(4):531. https://doi.org/10.1001/jamainternmed.2014.8063
Woods NF, Mitchell ES. Symptoms during the perimenopause: prevalence, severity, trajectory, and significance in women’s lives. Am J Med. 2005;118(12):14-24. https://doi.org/10.1016/j.amjmed.2005.09.031
Gold EB, Colvin A, Avis N, et al. Longitudinal analysis of the association between vasomotor symptoms and race/ethnicity across the menopausal transition: study of women’s health across the nation. Am J Public Health. 2006;96(7):1226-1235. https://doi.org/10.2105/AJPH.2005.066936
Goldstein LA, Jakubowski KP, Huang AJ, et al. Lifetime history of interpersonal partner violence is associated with insomnia among midlife women veterans. Menopause. 2023;30(4):370-375. https://doi.org/10.1097/GME.0000000000002152
Campbell SB, Renshaw KD. Posttraumatic stress disorder and relationship functioning: a comprehensive review and organizational framework. Clin Psychol Rev. 2018;65:152-162. https://doi.org/10.1016/j.cpr.2018.08.003
Assaf AR, Bushmakin AG, Joyce N, Louie MJ, Flores M, Moffatt M. The relative burden of menopausal and postmenopausal symptoms versus other major conditions: a retrospective analysis of the medical expenditure panel survey data. Am Health Drug Benefits. 2017;10(6):311-321.
Whiteley J, DiBonaventura M daCosta, Wagner JS, Alvir J, Shah S. The impact of menopausal symptoms on quality of life, productivity, and economic outcomes. J Womens Health (Larchmt). 2013;22(11):983-990. https://doi.org/10.1089/jwh.2012.3719
Street AE, Stafford J, Mahan CM, Hendricks A. Sexual harassment and assault experienced by reservists during military service: prevalence and health correlates. J Rehabil Res Dev. 2008;45(3):409-419. https://doi.org/10.1682/jrrd.2007.06.0088
Bromberger JT, Kravitz HM, Chang Y, et al. Does risk for anxiety increase during the menopausal transition? Study of women’s health across the nation. Menopause. 2013;20(5):488-495. https://doi.org/10.1097/GME.0b013e3182730599
Cohen LS, Soares CN, Vitonis AF, Otto MW, Harlow BL. Risk for new onset of depression during the menopausal transition: the Harvard Study of Moods and Cycles. Arch Gen Psychiatry. 2006;63(4):385. https://doi.org/10.1001/archpsyc.63.4.385
Bromberger JT, Epperson CN. Depression during and after the perimenopause: impact of hormones, genetics, and environmental determinants of disease. Obstet Gynecol Clin North Am. 2018;45(4):663-678. https://doi.org/10.1016/j.ogc.2018.07.007
Substance Abuse and Mental Health Services Administration. SAMHSA’s concept of trauma and guidance for a trauma-informed approach. HHS Publication No (SMA) 14–4884, Rockville, MD (2014) Substance Abuse and Mental Health Services Administrationhttps://ncsacw.acf.hhs.gov/userfiles/files/SAMHSA_Trauma.pdf (https://ncsacw.acf.hhs.gov/userfiles/files/SAMHSA_Trauma.pdf).
Evans GW, Li D, Whipple SS. Cumulative risk and child development. Psychol Bull. 2013;139(6):1342-1396. https://doi.org/10.1037/a0031808
Doucette CE, Morgan NR, Aronson KR, Bleser JA, McCarthy KJ, Perkins DF. The effects of adverse childhood experiences and warfare exposure on military sexual trauma among Veterans. J Interpers Violence. 2023;38(3-4):3777-3805. https://doi.org/10.1177/08862605221109494
Blosnich JR, Dichter ME, Cerulli C, Batten SV, Bossarte RM. Disparities in adverse childhood experiences among individuals with a history of military service. JAMA Psychiatry. 2014;71(9):1041. https://doi.org/10.1001/jamapsychiatry.2014.724
Aronson KR, Perkins DF, Morgan NR, et al. The impact of Adverse Childhood Experiences (ACEs) and combat exposure on mental health conditions among New Post-9/11 Veterans. Psychol Trauma: Theory, Res, Pract, Policy. 2020;12(7):698-706. https://doi.org/10.1037/tra0000614
Yano EM, Haskell S, Hayes P. Delivery of gender-sensitive comprehensive primary care to women veterans: implications for VA Patient Aligned Care Teams. J Gen Intern Med. 2014;29(S2):703-707. https://doi.org/10.1007/s11606-013-2699-3
Funding
This research was supported in part by VA Health Services Research & Career Development Award IK2 HX002402 (CJG), National Institute of Aging K24AG068601 (AJH), and VA Research Career Scientist Award IK6 CX002386 (ALB). The content is solely the responsibility of the authors and does not necessarily represent the official views of the Department of Veterans Affairs.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Dr. Gibson has served as an unpaid consultant to Astellas Pharmaceuticals for projects unrelated to the current manuscript. The authors have no other disclosures to report.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Prior presentations: Preliminary findings from this project were presented as part of a symposium. “Trauma and Health among Midlife and Aging Women,” at the American Psychosomatic Society 2022 Annual Meeting.
Rights and permissions
About this article
Cite this article
Travis, K.J., Huang, A.J., Maguen, S. et al. Military Sexual Trauma and Menopause Symptoms Among Midlife Women Veterans. J GEN INTERN MED 39, 411–417 (2024). https://doi.org/10.1007/s11606-023-08493-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-023-08493-w